Blood Test Numbers and What They Mean
If you have ever been confused by a blood test, you are not alone. Hopefully this breakdown helps you understand what your numbers mean.
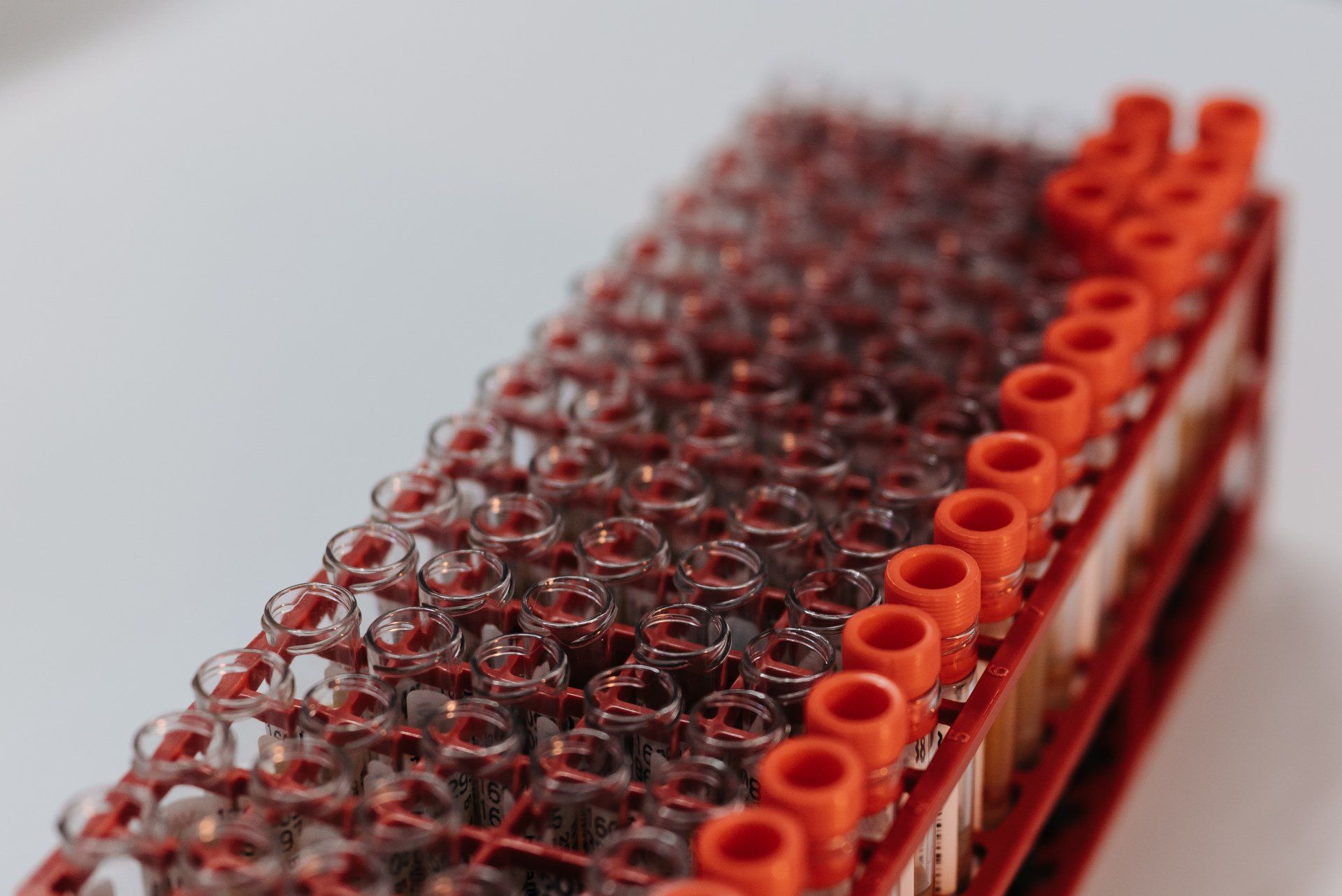
As we have learned more about our bodies over the years and technology has evolved, we are now able to find out a lot about how our bodies are functioning just by testing our blood for certain markers. Many insurances not only cover most blood work, but some require it as it is mutually beneficial to catch any possible issues early. It is not uncommon to receive the results of your blood work and see a page with large words and numbers that may seem more confusing than helpful. Below I do my best at a simple breakdown of different blood tests and what the different markers are. As with anything related to the body, none of these molecules work independently. They are all part of multiple complicated systems and should be treated that way. If you have concerns, you should contact a medical professional for clarification. If you've ever been confused by your blood test, hopefully this helps.

Complete Blood Count (CBC)
A CBC measures red blood cells (RBCs), white blood cells (WBCs), platelets, hematocrit, and hemoglobin. RBCs are responsible for delivering oxygen to tissues and removing carbon dioxide waste. WBCs are responsible for defending the body against infection. There are five types of WBCs: Neutrophils, Lymphocytes, Eosinophils, Basophils, Monocytes. A low WBC count can indicate being susceptible to infection (immunosuppressed), and a high WBC count can be a result of illness or an underlying medical condition. Platelets are responsible for part of wound healing and blood clotting. Hematocrit is the volume percentage of RBCs in your blood (compared to WBCs and plasma). Hemoglobin is a protein on red blood cells that is responsible for carrying oxygen to tissues and removing carbon dioxide. Current accepted values for these tests are below:
RBC:
Male: 4.35 - 5.65 trillion cells/L
Female: 3.92 - 5.13 trillion cells/L
WBC: 3.4 - 9.6 billion cells/L
Platelets:
Male: 135 - 317 billion cells/L
Female: 157 - 371 billion cells/L
Hematocrit:
Male: 38.3 - 48.6%
Female: 35.5 - 44.9%
Hemoglobin:
Male: 13.2 -16.6 grams/dL
Female: 11.6 -15 grams/dL
Comprehensive Metabolic Panel (CMP)
A CMP measures the level of many blood markers: Glucose, Calcium (Ca2+), Albumin, Protein, Sodium (Na+), Potassium (K+), Chloride (Cl-), Bicarbonate (HCO3-), Aspartate Aminotransferase (AST), Alkaline Phosphatase (ALP), Alanine Aminotransferase (ALT), Bilirubin, Blood Urea Nitrogen (BUN), and Creatinine. Glucose is the main sugar found in your blood and is used for energy by the cells. Calcium (Ca 2+) is an important mineral with many important functions including muscle contraction, nerve function, heart rhythm, and several others. Albumin is a plasma protein made in your liver that keeps fluid in your bloodstream (oncotic pressure) and prevents them from leaking into tissues. Albumin also acts as a transporter for ligands or drugs as they travel through your blood. Protein: There are several different categories of proteins that exist in the blood, one of which (the majority) is albumins. The others are Globulins, Fibrinogens, Regulatory Proteins, and Clotting Factors. Each family has a set of functions but the main ones deal with transporting hormones and other molecules as well as enzyme responsibilities. Sodium (Na+) is an electrolyte and mineral found in everything from table salt to aspirin. This ion is important for nerve and muscle function as well as maintaining proper fluid balances in your tissues. Potassium (K+), similar to the other electrolytes found here and throughout your body, plays a key role in regulating fluid levels in your tissues. Potassium has a close relationship with sodium and usually has opposing effects. For example, potassium is responsible for maintaining fluid levels inside the cells while sodium regulates levels outside of them. Improper fluid regulation can lead to blood pressure problems and ultimately a long list of possible cardiovascular issues. Chloride (Cl-) is another electrolyte responsible for fluid volume regulation as well as acid and base balancing. Bicarbonate (HCO3): Testing bicarbonate is another way to look at Carbon Dioxide levels in the body. Our blood brings bicarbonate to our lungs where it is exhaled as CO2. Bicarbonate has a negative charge on it and thus acts as a base in our body (high pH). Our body has two main ways to deal with regulating our blood pH, via the respiratory system (breathing rate), and the renal system (kidney function). Aspartate Aminotransferase (AST) is an enzyme found in muscles and in the liver. When the liver is damaged, AST is released into the bloodstream. Alkaline Phosphatase (ALP) is an enzyme mainly found in your liver and bones. High levels can be a sign of liver damage or possibly a bone disorder. Alanine Aminotransferase (ALT) is another enzyme found in the liver and high levels in the blood may reflect damage to the liver. Bilirubin is a yellowish byproduct of the breakdown of red blood cells. It is found in the bile in your liver. A healthy liver will remove most of the bilirubin, however, if the liver is not functioning properly, some of the yellow bilirubin can leak into the bloodstream and cause jaundice (yellowing of the skin and eyes). While not directly harmful, high bilirubin levels can be a sign of a malfunctioning liver. Blood Urea Nitrogen (BUN) measures the amount of nitrogen in your blood. In your body, proteins are broken down (produce ammonia which contains nitrogen) and ultimately produce urea in the liver. Urea then travels to the kidneys in the bloodstream where the waste should be filtered out and removed as urine. If the kidneys are not functioning properly, the urea may not be excreted properly and stay in the blood. Therefore, high urea levels may be an indication of a malfunctioning kidney. Creatinine is a byproduct of creatine breakdown during the energy producing process with ATP. Creatinine is then filtered out of the blood through the kidneys, eventually being excreted in your urine. Improper levels of creatinine can be a sign of kidney issues. One thing to keep in mind with creatinine levels is that creatine is a common supplement. When taking exogenous molecules into consideration, the clearance rate of creatinine can be more indicative of kidney function than the levels themselves. This is something that needs to be taken into consideration when looking at blood work and is one of many reasons why your doctor may ask you if you are taking any medications or supplements. Current accepted values for these tests are below:
Glucose: 70 - 100 mg/dL
Calcium: 8.5 - 10.2 mg/dL
Albumin: 3.4 - 5.4 g/dL
Protein: 6.0 - 8.3 g/dL
Sodium: 135 -145 mEq/L
Potassium: 3.7 - 5.2 mEq/L
Chloride: 96 - 106 mEq/L
Bicarbonate: 23 - 29 mEq/L
AST: 8 - 33 U/L
ALP: 20 - 130 U/L
ALT: 4 - 36 U/L
Bilirubin: 0.1 - 1.2 mg/dL
BUN: 6 - 20 mg/dL
Creatinine: 0.6 - 1.3 mg/dL
A lipid panel usually measures total cholesterol, LDL, HDL, and triglycerides. Total Cholesterol: Cholesterol moves through the body packaged into three main lipoproteins: HDL (High Density Lipoprotein), LDL (Low Density Lipoprotein), and VLDL (Very Low Density Lipoprotein). Unfortunately, cholesterol has gotten a bad reputation because chronic high levels can cause a multitude of circulatory issues. While in fact, cholesterol is a precursor for many of the essential hormones in our body as well as the production of vitamin D. Total Cholesterol test numbers usually reflect the sum of HDL, VLDL, and LDL. Low Density Lipoprotein (LDL) is often labeled as bad cholesterol. LDL molecules are made up of mostly cholesterol with triglycerides and proteins. Lipoproteins are necessary to transport these components because cholesterol and triglycerides exhibit fat-like properties when it comes to solubility. This simply means they are somewhat hydrophobic and require assistance, which is provided by the lipoprotein, to be circulated in the aqueous bloodstream. LDL has a greater protein to lipid ratio than VLDL and therefore is somewhat more dense. LDL plays a key role in transporting cholesterol to cells. LDL particles can be modified through processes in the body and become "oxidized" leading to OxLDL. There is a long history of research into the different modifications of LDL and their role in disease progression but the most common and simple explanation for why OxLDL is very bad is it is known to trigger the end stages of the progression of atherosclerosis which is dangerous and can lead to heart attack, stroke, and other cardiovascular diseases. High Density Lipoproteins (HDL) have less cholesterol than LDL and more protein and thus are a more dense molecule. HDL brings cholesterol from cells back to the liver and are sometimes termed "good cholesterol". Triglycerides: Triglycerides are a type of fat (lipid) that is both consumed and produced by the body. Both Triglycerides and Cholesterols are lipids, however, only triglycerides are fats. Most fats that we consume in our diet exist in the triglyceride form. Excess carbohydrates can also be converted to triglycerides by our liver. These molecules are usually stored in fat cells (adipose tissue) for later energy use. Triglycerides are great for energy storage because they do not require water and can therefore be densely packed. Current accepted values for these tests are below:
Total Cholesterol:
Normal: <200 mg/dL
High: >240 mg/dL
LDL:
Normal: <100 mg/dL
High: >160 mg/dL
HDL:
Low: <40 mg/dL
Normal: >60 mg/dL
Triglycerides:
Normal: <150 mg/dL
High: >200 mg/dL
HbA1c: HbA1c, A1C, glycosylated hemoglobin, and glycated hemoglobin are all tests to measure the percentage of hemoglobin that has a glucose (sugar) molecule attached to it. A1C levels can show how well a person has been controlling their blood sugar levels over approximately the previous three months. The higher your A1C level, the greater your risk for developing type 2 diabetes is. Current accepted values for these tests are below:
Normal: < 5.7%
Pre-diabetic: 5.7-6.4%
Diabetic: > 6.5%
C-Reactive Protein (hs-CRP)
hs-CRP: C-Reactive Protein is a protein produced by the liver in response to inflammation. Higher levels of CRP can be indicative of an inflammatory disorder but is largely nonspecific. CRP tests can measure levels greater than 3 mg/L while a hs-CRP test can detect values much smaller and are often used to look for risks of heart disease and stroke. Current accepted values for these tests are below:
CRP:
Normal: <10 mg/L
High: ≥ 10 mg/L
hs-CRP:
Low Risk: < 2 mg/L
High Risk: ≥ 2 mg/L
Vitamin D plays numerous roles in the body, far too many for me to explain here. Both Vitamin D2 and D3 are converted to 25 hydroxyvitamin D, which is what is measured during blood tests. Since this vitamin impacts so many biological pathways, having proper levels is important. Irregular levels can indicate nutritional problems, medical conditions, or bone disorders. The actual necessary levels may differ depending on each person's age, sex, and body composition. Current accepted values for these tests are below:
25-hydroxyvitamin D:
Normal: 20-40 ng/mL or 30-50 ng/mL
Iron/Ferritin
Iron/Ferritin: Ferritin is a protein in the blood that stores Iron. Higher ferritin levels usually reflect high levels of iron and vice versa. Current accepted values for these tests are below:
Ferritin:
Men: 24-336 µg/L
Women: 11-307 µg/L
Gamma-Glutamyl Transferase (GGT)
GGT is an enzyme found in the liver and can leak into the blood when the liver or the bile ducts become damaged. High levels are common amongst people who have an alcohol use disorder but can be indicative of other problems as well. Certain drugs such as phenobarbital can elevate GGT levels and therefore drug use needs to be taken into consideration when diagnosing liver issues this way. Current accepted values for these tests are below:
GGT (Adults):
Male: 8-61 U/L
Female: 5-36 U/L
Uric Acid is produced when purines are broken down. This is done mainly in the liver and kidneys as well as a few other areas. It is eliminated by the kidneys. There are many reasons why one may have an elevated uric acid level but a common concern is the development of arthritis and gout as well as kidney stones. Having too low of Uric Acid levels can also be harmful as it has been shown to play a role in immune responses. Current accepted values for these tests are below:
Uric Acid: 3.5 - 7.2 mg/dL
The somewhat simplified thyroid pathway begins in the hypothalamus, a section of the brain. The hypothalamus produces Thyrotropin-releasing hormone (TRH) which signals the release of Thyroid Stimulating Hormone (TSH) from the anterior pituitary. This TSH is released and signals the thyroid to increase thyroid hormone production. Thyroid hormone exists in two main forms triiodothyronine (T3) and thyroxine (T4), of which T4 is the main form found in the blood. The difference between T3 and T4 chemically speaking is three versus four iodine atoms attached to the main hormone. Both the hypothalamus and pituitary have T4 receptors which allows them to regulate the amount of TRH and TSH to produce respectively. If there is a high number of T4 in the blood, production of these other hormones is shut off. The majority of thyroid hormone in the blood is "bound" to protein. Only the free portion can enter tissues. Therefore blood tests usually test for both forms of the hormone. T4 and T3 exert their effects on a multitude of tissues and are therefore very important. The downside is that there are a lot of places that the system can go wrong so it is important to get these numbers checked if you are chronically feeling unwell. Current accepted values for these tests are below:
TSH Total: 0.5-5.0 mIU/L
T4 Total: 5-12 µg/dL
T4 Free: 0.7-1.9 ng/dL